STD's
What is Syphilis ?
Syphilis is a complex sexually transmitted disease (STD) caused by the bacterium Treponema Pallidum. It has often been called the great imitator because so many of the signs and symptoms are indistinguishable from those of other diseases.

How is syphilis spread ?
The syphilis bacterium is passed from person to person through direct contact with a syphilis sore. Sores mainly occur on the external genitals, vagina, anus, or in the rectum. Sores also can occur on the lips and in the mouth. Transmission of the organism occurs during vaginal, anal, or oral sex. Pregnant women with the disease can pass it to the babies they are carrying. Syphilis cannot be spread by toilet seats, door knobs, swimming pools, hot tubs, bath tubs, shared clothing, or eating utensils.
What are the signs and symptoms in adults ?
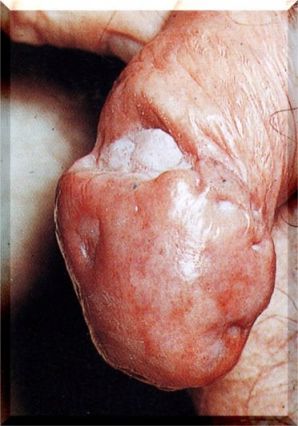
The time between picking up the bacterium and the start of the first symptom can range from 10-90 days (average 21 days). The primary stage of syphilis is marked by the appearance of a single sore (called a chancre). The chancre is usually firm, round, small, and painless. It appears at the spot where the bacterium entered the body. The chancre lasts 1-5 weeks and will heal on its own. If adequate antibiotic treatment is not administered, the infection progresses to the secondary stage.
The second stage starts when one or more areas of the skin break into a rash that usually does not itch. Rashes can appear as the chancre is fading or can be delayed for weeks. The rash often appears as rough, "copper penny" spots on both the palms of the hands and the bottoms of the feet. The rash also may appear as a prickly heat rash, as small blotches or scales all over the body, as a bad case of old acne, as moist warts in the groin area, as slimy white patches in the mouth, as sunken dark circles the size of a nickel or dime, or as pus-filled bumps like chicken pox. Some of these signs on the skin look like symptoms of other diseases.

Sometimes the rashes are so faint they are not noticed. Rashes typically last 2-6 weeks and clear up on their own. In addition to rashes, second stage symptoms can include fever, swollen lymph glands, sore throat, patchy hair loss, headaches, weight loss, muscle aches, and tiredness. A person can easily pass the disease to sex partners when first or second stage signs or symptoms are present without realizing it.
The latent (hidden) stage of syphilis begins when the secondary symptoms disappear. If the infected person has not received antibiotic treatment, he/she still has syphilis even though there are no signs or symptoms. The bacterium remains in the body and begins to damage the internal organs, including the brain, nerves, eyes, heart, blood vessels, liver, bones, and joints. In about one-third of untreated persons, this internal damage shows up many years later in the late or tertiary stage of syphilis. Late stage signs and symptoms include not being able to coordinate muscle movements, paralysis, no longer feeling pain, gradual blindness, dementia (madness) or other personality changes, impotency, shooting pains, blockage or ballooning of the heart vessels, tumors or "gummas" on the skin, bones, liver, or other organs, severe pain in the belly, repeated vomiting, damage to knee joints, and deep sores on the soles of the feet or toes. This damage may be serious enough to cause death.
Can a newborn get syphilis ?
An infected pregnant woman has about a 40% chance of having a stillbirth (syphilitic stillbirth) or giving birth to a baby who dies shortly after birth. A baby born to a mother with either untreated syphilis or syphilis treated after the 34th week of pregnancy has a 40% - 70% chance of being infected with syphilis (congenital syphilis). An infected baby may be born without symptoms but may develop them within a few weeks, if not treated immediately. These signs and symptoms can be very serious and include skin sores, a very runny nose, which is sometimes bloody (and infectious), slimy patches in the mouth, inflamed arm and leg bones, a swollen liver, anemia, jaundice, or a small head. Untreated babies may become retarded or may have seizures. About 12% of infected newborns will die because of the disease.
How is syphilis diagnosed ?
The syphilis bacterium can be detected by a health care provider who examines material from infectious sores under a microscope. Shortly after infection occurs, the body produces syphilis antibodies that are detected with a blood test. A syphilis blood test is accurate, safe, and inexpensive. A low level of antibodies will stay in the blood for months or years after the disease has been successfully treated, and antibodies can be found by subsequent blood tests. Because untreated syphilis in a pregnant woman can infect and possibly kill her developing baby, every pregnant woman should have a blood test for syphilis.

How common is syphilis ?
In the United States, nearly 38,000 cases of syphilis were detected by health officials in 1998, including 7,000 cases of primary and secondary syphilis and 800 cases of congenital syphilis in newborns. More cases occur each year than come to the attention of health officials. The eight states with the highest 1998 syphilis rates were located in the southern region of the U.S. These states had rates 2-5 times higher than the national rate. In 1998, 28 counties accounted for 50% of all primary and secondary syphilis cases. Three hundred twelve counties had syphilis rates greater than the Year 2000 objective of 4 cases per 100,000. Ninety- one percent of these were in the South.
In 1998, syphilis occurred primarily in persons aged 20 to 39 and slightly more frequently in males than females. Syphilis rates in females were higher in the 20-24 age group, while male rates were higher in the 30 to 39 age group. Some fundamental societal problems, such as poverty, inadequate access to health care, and lack of education are associated with disproportionately high levels of syphilis in certain populations. Cases in 1998 had the following race or ethnicity distribution: African-Americans 80%, whites 13%, Hispanics 6%, and others 1%. Syphilis is one of the most glaring examples of racial disparity in health status, with the rate for African-Americans nearly 34 times the rate for whites.

What is the link between syphilis and HIV ?
While the health problems caused by the syphilis bacterium for adults and newborns are serious in their own right, it is now known that the genital sores caused by syphilis in adults also make it easier to transmit and acquire HIV infection sexually. There is a 2- to 5-fold increased risk of acquiring HIV infection when syphilis is present. Areas of the U.S. that have the highest rates of syphilis also have the fastest-growing HIV infection rates in women of childbearing age.
Is there a cure or treatment for syphilis ?
The antibiotic penicillin or doxycycline will cure a person who has had syphilis for less than a year. More doses are needed to cure someone who has had it for longer than a year. A baby born with the disease needs daily penicillin or doxycycline treatment for 10 days. There are no home remedies or over-the-counter drugs that cure syphilis. Penicillin and doxycycline treatment will kill the syphilis bacterium and prevent further damage, but it will not repair any damage already done.
Penicillin, a common antibiotic, is no longer the antibiotic of choice to treat syphilis, because some strains of the syphilis bacterium have become resistant to penicillin.
Persons who receive syphilis treatment must abstain from sexual contact with new partners until the syphilis sores are completely healed. Persons with syphilis must notify their sex partners so that they also can receive treatment because who have been treated can also get the disease again if they have sexual contact with an infected person. For this reason both partners should be treated at the same time, even if the other person has no symptoms.
The most common regiment prescribed by doctors would consist of 1, 100mg capsule every 12 hours (2x daily) for 7-10 days. 20 doxycycline capsules would be needed for one person. A stronger regiment for some STD's would consist of 1, 100mg capsule every 8 hours (3x daily) for 10-14 days. 42 doxycycline capsules would be needed to treat one person. This regiment is the most effective.
Will syphilis recur ?
Having had syphilis does not protect a person from getting it again. Antibodies are produced as a person reacts to the disease, and, after treatment, these antibodies may offer partial protection from getting infected again, if exposed right away. Even though there may be a short period of protection, the antibody levels naturally decrease in the blood, and people become susceptible to syphilis infection again if they are sexually exposed to syphilis sores.
How can people protect themselves against infection ?
Two people who know they are not infected and who have sex with no one
but each other cannot contract syphilis. When a person has sex with a
person whose syphilis status is unknown, a latex condom put on before
beginning sex and worn until the penis is withdrawn is a good defense
against infection. Only lab tests can confirm whether someone has syphilis.
Because syphilis sores can be hidden in the vagina, rectum, or mouth,
it may not be obvious that a sex partner has syphilis. Washing the genitals,
urinating, or douching after sex does not prevent STDs, including syphilis.
Any unusual discharge, sore, or rash, especially in the groin area, should
be a signal to stop having sex and to see a doctor at once.
What causes gonorrhea ?
Gonorrhea is caused by Neisseria gonorrhoeae, a bacterium that can grow and multiply easily in mucous membranes of the body. Gonorrhea bacteria can grow in the warm, moist areas of the reproductive tract, including the cervix (opening to the womb), uterus (womb), and fallopian tubes (egg canals) in women, and in the urethra (urine canal) in women and men. The bacteria can also grow in the mouth, throat, and anus.
How do people get gonorrhea ?
Gonorrhea is spread through sexual contact (vaginal, oral, or anal). This includes penis-to- vagina, penis-to-mouth, penis-to-anus, mouth-to-vagina, and mouth-to-anus contact. Ejaculation does not have to occur for gonorrhea to be transmitted or acquired. Gonorrhea can also be spread from mother to child during birth.
Gonorrhea infection can spread to other unlikely parts of the body. For example, a person can get an eye infection after touching infected genitals and then the eyes. Individuals who have had gonorrhea and received treatment may get infected again if they have sexual contact with persons infected with gonorrhea.

How common is gonorrhea ?
Gonorrhea is a very common infectious disease. Each year approximately 650,000 people in the United States are infected with gonorrhea. In 1998, the rate of reported gonorrhea infections was 132.9 per 100,000 persons.
What are the signs and symptoms of gonorrhea ?
When initially infected, about 50% of men have some signs or symptoms. Symptoms and signs include a burning sensation when urinating and a yellowish white discharge from the penis. Sometimes men with gonorrhea get painful or swollen testicles.
In women, the early symptoms of gonorrhea are often mild, and many women who are infected have no symptoms of infection. Even when a woman has symptoms, they can be so non-specific as to be mistaken for a bladder or vaginal infection. The initial symptoms and signs in women include a painful or burning sensation when urinating and a vaginal discharge that is yellow or bloody. Women with no or mild gonorrhea symptoms are still at risk of developing serious complications from the infection. Untreated gonorrhea in women can develop into pelvic inflammatory disease (PID). Please see below for the complications of gonorrhea.

Symptoms of rectal infection include discharge, anal itching, soreness, bleeding, and sometimes painful bowel movements. Infections in the throat cause few symptoms.
When do symptoms appear ?
In males, symptoms usually appear 2 to 5 days after infection, but it can take as long as 30 days for symptoms to begin. Regardless of symptoms, once a person is infected with gonorrhea, he or she can spread the infection to others if condoms or other protective barriers are not used during sex.
How is gonorrhea diagnosed ?
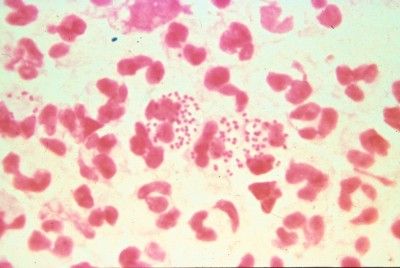
Several laboratory tests are available to diagnose gonorrhea. A health care provider can obtain a sample of fluid from the infected mucus membrane (cervix, urethra, rectum, or throat) and send the specimen to a laboratory for analysis. Gonorrhea that is present in the male or female genital tract can be diagnosed in a laboratory by using a urine specimen from an infected person. A quick laboratory test for gonorrhea that can be done in the clinic or doctor’s office is a Gram stain. The Gram stain allows the doctor to see the gonorrhea bacteria under a microscope. This test works better for men than for women.
Who is at risk for gonorrhea ?
Any sexually active person can be infected with gonorrhea. In the United States, approximately 75% of all reported gonorrhea is found in younger persons aged 15 to 29 years. The highest rates of infection are usually found in 15- to 19-year-old women and 20- to 24-year-old men. In 1998, approximately 1 of every 30 African American youths aged 15 to 24 had gonorrhea.

What is the treatment for gonorrhea ?
The antibiotic Doxycycline can successfully cure uncomplicated gonorrhea in adolescents and adults. Penicillin is a common antibiotic that is no longer used to treat gonorrhea, because many strains of the gonorrhea bacterium have become resistant to penicillin. Persons with gonorrhea should also be screened for other STDs. The most common regiment prescribed by doctors would consist of 1, 100mg capsule every 12 hours (2x daily) for 7-10 days. 20 doxycycline capsules would be needed for one person. A stronger regiment for some STD's would consist of 1, 100mg capsule every 8 hours (3x daily) for 10-14 days. 42 doxycycline capsules would be needed to treat one person. This regiment is the most effective. If you think you are infected, avoid sexual contact and seek immediate medical attention and treatment.
It is important to take all of the medication prescribed to cure gonorrhea, even if the symptoms or signs stop before all the medication is gone. Although medication will stop the infection, it will not repair any permanent damage done by the disease. Persons who have had gonorrhea and have been treated can also get the disease again if they have sexual contact with an infected person. For this reason both partners should be treated at the same time, even if the other person has no symptoms.
What are the complications of gonorrhea ?
Untreated gonorrhea can cause serious and permanent problems in both women and men.
In women, gonorrhea is a common cause of pelvic inflammatory disease (PID). About 1 million women each year in the United States develop PID. Women with PID do not necessarily have symptoms or signs. When symptoms or signs are present, they can be very severe and can include strong abdominal pain and fever. PID can lead to internal abscesses (pus pockets that are hard to cure), long-lasting pelvic pain, and infertility. PID can cause infertility or damage the fallopian tubes (egg canals) enough to increase the risk of ectopic pregnancy. Ectopic pregnancy is a life-threatening condition in which a fertilized egg grows outside the uterus, usually in a fallopian tube.
In men, gonorrhea can cause epididymitis, a painful condition of the testicles that can sometimes lead to infertility if left untreated. Without prompt treatment, gonorrhea can also affect the prostate and can lead to scarring inside the urethra, making urination difficult.
Gonorrhea can spread to the blood or joints. This condition can be life-threatening. Also, persons with gonorrhea can more easily contract HIV, the virus that causes AIDS. Persons with HIV infection and gonorrhea are more likely than persons with HIV infection alone to transmit HIV to someone else.
How does gonorrhea affect a pregnant woman and her baby ?
Gonorrhea in a pregnant woman can cause premature delivery or spontaneous abortion. The infected mother may give the infection to her infant as the baby passes through the birth canal during delivery. This can cause bldness, joint infection, or a life-threatening blood infection in the baby. Treatment of gonorrhea as soon as it is detected in pregnant women will lessen the risk of these complications. Pregnant women should consult a health care provider for appropriate medications.
How can gonorrhea be prevented ?
Use latex condoms correctly every time you have sex.
Persons who choose to engage in sexual behaviors that can place them at risk for STDs should use latex condoms every time they have sex. A condom put on the penis before starting sex and worn until the penis is withdrawn can help protect both the male and the female partner from gonorrhea. When a male condom cannot be used appropriately, sex partners should consider using a female condom.
Condoms do not provide complete protection from all STDs. Sores and lesions of other STDs on infected men and women may be present in areas not covered by the condom, resulting in transmission of infection to another person.
Limit the number of sex partners, and do not go back and forth between partners. Practice sexual abstinence, or limit sexual contact to one uninfected partner.
If you think you are infected, avoid sexual contact and seek immediate medical attention and treatment. Persons who have had chlamydia and have been treated can also get the disease again if they have sexual contact with an infected person. For this reason both partners should be treated at the same time, even if the other person has no symptoms.
Any genital symptoms such as discharge or burning during urination or unusual sore or rash should be a signal to stop having sex and to consult a health care provider immediately. If you are told you have gonorrhea or any other STD and receive treatment, you should notify all of your recent sex partners so that they can see a health care provider and be treated. This will reduce the risk that your partners will develop serious complications from gonorrhea and will reduce your own risk of becoming reinfected.
What is Chlamydia ?
Chlamydia is a sexually transmitted disease (STD) that is caused by the bacterium Chlamydia trachomatis. Because approximately 75% of women and 50% of men have no symptoms, most people infected with Chlamydia are not aware of their infections and therefore may not seek health care.
When diagnosed, Chlamydia can be easily treated and cured. Untreated, Chlamydia can cause severe, costly reproductive and other health problems which include both short- and long-term consequences, including pelvic inflammatory disease (PID), which is the critical link to infertility, and potentially fatal tubal pregnancy.
Up to 40% of women with untreated Chlamydia will develop PID. Undiagnosed PID caused by Chlamydia is common. Of those with PID, 20% will become infertile; 18% will experience debilitating, chronic pelvic pain; and 9% will have a life-threatening tubal pregnancy. Tubal pregnancy is the leading cause of first-trimester, pregnancy-related deaths in American women.
Chlamydia may also result in adverse outcomes of pregnancy, including neonatal conjunctivitis and pneumonia. In addition, recent research has shown that women infected with Chlamydia have a 3 - 5 fold increased risk of acquiring HIV, if expose
Chlamydia is also common among young men, who are seldom offered screening. Untreated Chlamydia in men typically causes urethral infection, but may also result in complications such as swollen and tender testicles.
What is the magnitude of the problem ?
Chlamydia is the most frequently reported infectious disease in the United States. Though 526,653 cases were reported in 1997, an estimated 3 million cases occur annually. Severe under reporting is largely a result of substantial numbers of asymptomatic persons whose infections are not identified because screening is not available. Highlights of reported data are as follows:
· From 1984 through 1997, reported rates(1) of Chlamydia increased from 3.2 to 207.0 cases per 100,000 population. This trend primarily reflects increased screening, recognition of asymptomatic infection (mainly in women), and improved reporting capacity rather than a true increase in disease incidence.
· In 1997, the reported rate of Chlamydia for women (335.8) substantially exceeded the rate for men (70.4), due mainly to increased detection of asymptomatic infection in women through screening. Low rates of reported Chlamydia among men suggest that many of the partners of women with Chlamydia are not screened or treated.

· As in previous years, 1997 rates of Chlamydia were highest in the West and the Midwest, where substantial resources have been committed for organized screening programs.
What are the symptoms of Chlamydia ?
The symptoms of early-stage Chlamydia are usually nonexistent for four out of five women. The most common symptom, if any, is increased or abnormal vaginal discharge, which usually develops about fourteen days after infection. Sometimes a strong, rather foul vaginal odor develops as well. Painful urination, unusual vaginal bleeding, bleeding after sex, and low abdominal pain may also be signs, and the cervix may become inflamed (noticeable when you are examined by a doctor). If your cervix bleeds easily after a Pap smear, this is also a major clue. If Chlamydia spreads to your uterus and fallopian tubes, it will have progressed to PID, and you may develop some of the symptoms discussed below.
Men, like women, may have pain during urination, or they may notice a burning and itching around or discharge from the penis or pain and swelling in the testicles. Chlamydia is a very insidious disease because it rarely causes symptoms. People don't know they're infected so they don't get treated. Then they infect their partners who also don't get treated.

One way to find out whether you have Chlamydia is to ask your partner whether he has symptoms of NGU. Painful urination or urethral discharge that appear one to three weeks after infection are telltale signs. About 10 percent of the time, men show no symptoms of Chlamydia either. Chlamydia can now be detected in men through a simple urine test. The best thing you can do if you're sexually active is to be regularly screened for Chlamydia by your family doctor. The test is 90 percent accurate. The screening is simple: Your doctor takes a culture swab of cervical mucus. It can be done in conjunction with a Pap test. How regularly should you be swabbed? Every time you have a new partner. If you test negative but still suspect it, request antibiotic treatment for it anyway. Even if you are treated for nonexistent Chlamydia, the treatment is relatively harmless to you, other than the mild side effects of antibiotics discussed below.

What is the treatment for Chlamydia ?
The good news about Chlamydia is that it is extremely easy to treat. Doxycycline will cure both Chlamydia and ureaplasma infections. Two Doxycycline 100mgs capsules per day for ten days in most cases will cure Chlamydia. Penicillin, on the other hand, is not effective here. Penicillin is a common antibiotic that is no longer used to treat Chlamydia, because many strains of the Chlamydia bacterium have become resistant to penicillin. If you think you are infected, avoid sexual contact and seek immediate medical attention and treatment.
It is important to take all of the medication prescribed to cure Chlamydia, even if the symptoms or signs stop before all the medication is gone. Persons who have had Chlamydia and have been treated can also get the disease again if they have sexual contact with an infected person. For this reason both partners should be treated at the same time, even if the other person has no symptoms.
A normal prescription would consist of 1, 100mg capsule every 12 hours (2x daily) for 7-10 days. 20 Doxycycline capsules would be needed for one person. A stronger regiment for some STD's would consist of 1, 100mg capsule every 8 hours (3x daily) for 10-14 days. 42 Doxycycline capsules would be needed to treat one person. This is the most effective regiment.
How does Chlamydia affect a pregnant woman and her baby ?
As many as 10 percent of all pregnant women are believed to be infected with Chlamydia. This can lead to all kinds of complications during pregnancy or at birth, including miscarriage, infant pneumonia, infant conjunctivitis (severe eye infection), and even infant blindness. If you're pregnant, request a screening for Chlamydia as soon as you can. Treatment of Chlamydia as soon as it is detected in pregnant women will lessen the risk of these complications. Pregnant women should consult a health care provider for appropriate medications. The antibiotics should be taken as prescribed, or the infection could resurface. After you've finished your antibiotics, you will need to be rescreened to make sure that the infection is gone. Abstain from all sexual activity until you're sure that you are cured.
How can Chlamydia be prevented ?
Use latex condoms correctly every time you have sex.
Persons who choose to engage in sexual behaviors that can place them at risk for STDs should use latex condoms every time they have sex. A condom put on the penis before starting sex and worn until the penis is withdrawn can help protect both the male and the female partner from gonorrhea. When a male condom cannot be used appropriately, sex partners should consider using a female condom.
Condoms do not provide complete protection from all STDs. Sores and lesions of other STDs on infected men and women may be present in areas not covered by the condom, resulting in transmission of infection to another person.
Limit the number of sex partners, and do not go back and forth between partners. Practice sexual abstinence, or limit sexual contact to one uninfected partner.
If you think you are infected, avoid sexual contact and seek immediate medical attention and treatment. Persons who have had Chlamydia and have been treated can also get the disease again if they have sexual contact with an infected person. For this reason both partners should be treated at the same time, even if the other person has no symptoms.
Any genital symptoms such as discharge or burning during urination or unusual sore or rash should be a signal to stop having sex and to consult a health care provider immediately. If you are told you have Chlamydia or any other STD and receive treatment, you should notify all of your recent sex partners so that they can see a health care provider and be treated. This will reduce the risk that your partners will develop serious complications from Chlamydia and will reduce your own risk of becoming reinfected.
A final note on Chlamydia
The best way to avoid Chlamydia is to practice safe sex. It is also believed that hormonal contraceptives increase your risks of exposure because the cervical mucus changes and is therefore a better "host" for Chlamydia. The most disturbing fact about Chlamydia is that it is a leading cause of infertility. Physicians believe that if more attention were paid to preventing Chlamydia, infertility clinics would lose revenue, and the infertility "epidemic" going on today in North America would dramatically decrease.
Genital herpes
Genital herpes is usually the result of HSV-2 with about 10%
of cases being the result of HSV-1.

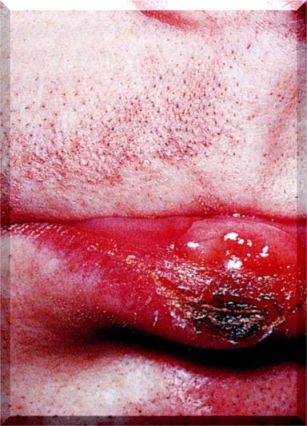
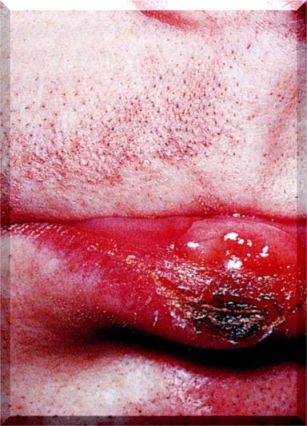
Primary infection is often asymptomatic but many painful lesions can develop on the glans or shaft of the penis in men

and on the vulva, vagina, cervix and perianal region of women
).
In both sexes, the urethra can be involved. In women, the infection may be accompanied by vaginal discharge.
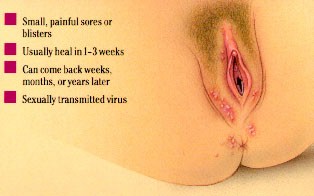
Genital herpes infections, which involve a transient viremia, can be accompanied by a variety of symptoms including fever, myalgia, glandular inflammation of the groin area (inguinal adenitis).

Secondary episodes of genital herpes, which occur as a result of reactivation of virus in the sacral ganglion, are frequently less severe (and last a shorter time) than the first episode. Recurrent episodes seem usually to result from a primary HSV-2 infection.


Patients who are about to experience a recurrence usually first experience a prodrome in which there is a burning sensation in the area that is about to erupt
.
HSV proctitis
This is an inflammation of the rectum and the anus
Some patients have only infrequent recurrences but others experience
recurrences as often as every 14-21 days. Whether there is an apparent
active disease or not, an infected patient remains infectious without
overt symptoms. Clearly, these persons are very important in the spread
of herpes infection.
What is pelvic inflammatory disease (PID) ?
Aside from AIDS, the most common and serious complication of sexually transmitted diseases (STDs) among women is pelvic inflammatory disease (PID), an infection of the upper genital tract. PID can affect the uterus, ovaries, fallopian tubes, or other related structures. Untreated, PID causes scarring and can lead to infertility, tubal pregnancy, chronic pelvic pain, and other serious consequences. Each year in the United States, more than 1 million women experience an episode of acute PID, with the rate of infection highest among teenagers. More than 100,000 women become infertile each year as a result of pelvic inflammatory diseases, and a large proportion of the 70,000 ectopic (tubal) pregnancies occurring every year are due to the consequences of PID. In 1997 alone, an estimated $7 billion was spent on pelvic inflammatory diseases and its complications.
What is the cause pelvic inflammatory disease (PID) ?
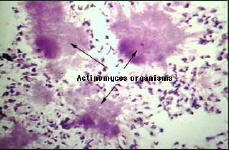
PID occurs when disease-causing organisms migrate upward from the urethra and cervix into the upper genital tract. Many different organisms can cause pelvic inflammatory diseases, but most cases are associated with gonorrhea and genital chlamydial infections, two very common STDs. Scientists have found that bacteria normally present in small numbers in the vagina and cervix also may play a role. Investigators are learning more about how these organisms cause PID. The gonococcus, Neisseria gonorrhea, probably travels to the fallopian tubes, where it causes sloughing (casting out) of some cells and invades others. Researchers think it multiplies within and beneath these cells. The infection then may spread to other organs, resulting in more inflammation and scarring. Chlamydia trachomatis and other bacteria may behave in a similar manner. Researchers do not know how other bacteria that normally inhabit the vagina (e.g., organisms such as Gardnerella vaginalis and Bacteroides) gain entrance into the upper genital tract. The cervical mucus plug and secretions may help prevent the spread of microorganisms to the upper genital tract, but it may be less effective during ovulation and menses. In addition, the gonococcus may gain access more easily during menses, if menstrual blood flows backward from the uterus into the fallopian tubes, carrying the organisms with it. This may explain why symptoms of pelvic inflammatory disease caused by gonorrhea often begin immediately after menstruation as opposed to any other time during the menstrual cycle. It is noteworthy that the co-incidence of menses and chlamydial infection is not a prominent feature of chlamydial PID. Bacteria normally found in the intestines that get into the pelvic cavity. This most likely happens:
After sexual intercourse, especially having vaginal intercourse right after having anal intercourse
After getting an intrauterine device (IUD) put in or repositioned (low risk)
Because of high-risk sexual practices that increase the risk of infection, such as having multiple sex partners or having sex with a person who has many partners
Having had PID in the past or a recent bout with vaginitis
What are the symptoms of PID ?
The major symptoms of pelvic inflammatory disease are lower abdominal pain and abnormal vaginal discharge. Other symptoms such as fever, pain in the right upper abdomen, painful intercourse, and irregular menstrual bleeding can occur as well. PID, particularly when caused by chlamydial infection, may produce only minor symptoms or no symptoms at all, even though it can seriously damage the reproductive organs.
Symptoms of Acute PID:
Pain in the abdomen or back (can be severe)
Bad-smelling vaginal discharge
Pain during intercourse
Abdominal tenderness and/or bloating
Difficult menstrual cramps
High fever
Symptoms of Chronic PID:
Pain (less severe) - often occurs halfway through the menstrual cycle or during a pelvic exam
Skin on abdomen is sensitive
Vaginal discharge
Change in menstrual flow
Nausea
Low-grade fever
What are the risk factors for PID ?
Women with STDs – especially gonorrhea and chlamydial infection – are at greater risk of developing PID; a prior episode of PID increases the risk of another episode because the body’s defenses are often damaged during the initial bout of upper genital tract infection. Sexually active teenagers are more likely to develop PID than are older women. The more sexual partners a woman has, the greater her risk of developing PID. Recent data indicate that women who douche once or twice a month may be more likely to have PID than those who douche less than once a month. Douching may push bacteria into the upper genital tract. Douching also may ease discharge caused by an infection, so the woman delays seeking health care.
What is the diagnosis for pelvic inflammatory diseases ?
PID can be difficult to diagnose. If symptoms such as lower abdominal pain are present, the doctor will perform a physical exam to determine the nature and location of the pain. The doctor also should check the patient for fever, abnormal vaginal or cervical discharge, and evidence of cervical chlamydial infection or gonorrhea. If the findings of this exam suggest that PID is likely, current guidelines advise doctors to begin antibiotic treatment. If more information is necessary, the doctor may order other tests, such as a sonogram, endometrial biopsy, or laparoscopy to distinguish between PID and other serious problems that may mimic PID. Laparoscopy is a surgical procedure in which a tiny, flexible tube with a lighted end is inserted through a small incision just below the navel. This procedure allows the doctor to view the internal abdominal and pelvic organs, as well as take specimens for cultures or microscopic studies, if necessary. Pelvic inflammatory diseases may be detected only later when they have trouble becoming pregnant and find that their reproductive organs have been damaged. PID may also be detected at a later time when a woman develops problems with pelvic pain.
What is the treatment for PID ?
Because culture of specimens from the upper genital tract are difficult to obtain and because multiple organisms may be responsible for an episode of PID, especially if it is not the first one, the doctor will prescribe either one or two antibiotics that are effective against a wide range of infectious agents. The symptoms may go away before the infection is cured. Even if symptoms do go away, patients should finish taking all of the antibiotics. Many women with PID have sex partners who have no symptoms, although their sex partners may be infected with organisms that can cause pelvic inflammatory diseases. Because of the risk of reinfection, however, sex partners should be treated even if they do not have symptoms. Treatment for PID is antibiotics (sometimes more than one kind over a period of 3-4 weeks) and bed rest. If the infection is severe or if vomiting is present, intravenous (IV) antibiotics may need to be given in a hospital. Preventing further infections is important. This may include treatment for an infected sex partner so as not to get reinfected. When pelvic inflammatory diseases are not treated, it can lead to blood poisoning, blood clots that break off and travel to the lungs, and bands of scar tissue in the pelvis. All of these can be life-threatening. Permanent damage to a woman's reproductive organs and/or infertility can occur as well.
Regimen A
Doxycycline - (100 mg) twice a day for 14 days.
Regimen B
Ceftriaxone - is given one time as a shot (250 mg) in a muscle.
Plus:
Doxycycline - (100 mg) twice a day for 14 days.
Other regiments are also used.
Click Here
Doxycycline Prices
What should I know about taking the antibiotic doxycycline ?
Take each dose with a full glass of water (8 ounces). Doxycycline may be taken with food or milk or on an empty stomach. Take all of the doxycycline that has been prescribed for you even if you begin to feel better. Your symptoms may start to improve before the infection is completely treated. Do NOT take antacids that contain magnesium or aluminum (e.g., Tums or Rolaids), the ulcer medicine sucralfate (Carafate), or vitamin or mineral supplements that contain iron or zinc for a minimum of 6 hours before or 2 hours after a dose of doxycycline. Taking antacids, sucralfate, or vitamin or mineral supplements too close to a dose of doxycycline can greatly decrease the effects of the antibiotic. Children younger than 8 years of age should NOT take doxycycline. It can cause permanent tooth discoloration, and it can affect growth. Do NOT BREAST-FEED while taking this medicine. Doxycycline may affect bone and tooth development in the developing baby. Do NOT take this medication without first talking to your doctor if you are pregnant. Doxycycline may DECREASE the effectiveness of birth control pills. Use a second method of birth control to prevent pregnancy while taking doxycycline.
What are the consequences of PID ?
Women with recurrent episodes of PID are more likely than women with a single episode to suffer scarring of the tubes that leads to infertility, tubal pregnancy, or chronic pelvic pain. Infertility occurs in approximately 20 percent of women who have had an pelvic inflammatory disease. Most women with tubal infertility, however, never have had symptoms of PID. Organisms such as C. trachomatis can silently invade the fallopian tubes and cause scarring, which blocks the normal passage of eggs into the uterus. A women who has had a pelvic inflammatory disease has a six-to-tenfold increased risk of tubal pregnancy, in which the egg can become fertilized but cannot pass into the uterus to grow. Instead, the egg usually attaches in the fallopian tube, which connects the ovary to the uterus. The fertilized egg cannot grow normally in the fallopian tube. This type of pregnancy is life-threatening to the mother, and almost always fatal to her fetus. It is the leading cause of pregnancy-related death in African-American women. In addition, untreated PID can cause chronic pelvic pain and scarring in about 20 percent of patients. These conditions are difficult to treat but are sometimes improved with surgery. Another complication of PID is the risk of repeated attacks of PID. As many as one-third of women who have had PID will have the disease at least one more time. With each episode of reinfection, the risk of infertility is increased.
What is prostatitis ?
Prostatitis is a persistent disease that causes pain and discomfort for many men. The term "prostatitis" refers to inflammation of the prostate gland. It can be debilitating, demoralizing and depressing. "Chronic prostatitis" refers to persistent inflammation and ongoing, long-term discomfort or pain. With it may occur the frequent urge to urinate or difficulty in urinating, burning during or after urination, and various sexual problems (including reduced erections, premature ejaculation, or pain during or after ejaculation). If you have been diagnosed with prostatitis or think you may have it, you are not alone. It has been estimated that, at some point in their lives, more than half of all men have some trouble with their prostate gland. Many are never diagnosed as such, because they choose to suffer in silence, or fortunately, there is not enough irritation to be recognized as a prostate problem or to seek treatment. In the higher age groups, the incidence of prostatitis rises significantly. It used to be that prostatitis was regarded as "an old man's disease", but it seems increasingly to be plaguing younger men; even many in their twenties and thirties. And increasingly, men with prostatitis are reaching out for help. There is no need to be embarrassed about having the problem. Many others have it too. And if no treatment is sought, there is far less chance of relief.
What are the symptoms of prostatitis ?
You may only have one symptom or they may happen in combination.
PAIN
1. Lower back
2. Lower abdomen
3. Groin and/or testicles
4. Around the perineum
URINARY SYMPTOMS
1. Gradual narrowing of the urinary tract manifested as splitting or dribbling of urine.
2. Occasional burning or itchy sensation during urination.
3. Increasing frequency and getting up at night to urinate.
4. Sensation of incomplete emptying of urine.
5. Difficulty in initiating urination.
6. Urinary obstruction.
SEXUAL DYSFUNCTION
1. Gradual diminution of erection or inability to maintain it.
2. Fast ejaculation.
3. Burning or itchy sensation during or after ejaculation.
4. Bloody or watery semen.
5. Diminished volume of semen or dry ejaculation.
6. Impotence.
How is prostatitis acquired ?
When bacteria from your urethra enters the prostate through a duct that connects the two, you can develop prostatitis. Putting unsterile toys or other objects into your urethra, or neglecting a urinary tract infection or urethritis (a sexually transmitted infection in your urethra) increases your chances of prostate infection. You can develop chronic prostatitis from oral or anal sex and even from an acute infection that was not completely cured, or from a mild infection that you probably never knew existed.
What are the treatments for prostatitis ?
Antibiotics may be prescribed for men with:
Acute bacterial prostatitis.
Chronic bacterial prostatitis.
In the USA, Canada, and much of Europe, your doctor is likely to treat you by prescribing antibiotics such as doxycycline or cipro which are fluoroquinolones. This is often done whether or not a culture of your EPS or semen is performed. The antibiotics may help if your prostatitis is caused by bacteria, or it may help due to anti-inflammatory effects of these antibiotics. Fluoroquinolone antibiotics are often prescribed immediately to treat prostatitis, before test results are available. If you begin to get better while taking cipro or doxycycline, the treatment is continued. If not, more tests will be done.
Trimethoprim/sulfamethoxazole (TMP/SMX) has been the standard therapy for prostatitis and has a cure rate of 30% to 50%. The new fluoroquinolones are rapidly replacing TMP/SMX for treating bacterial prostatitis. Fluoroquinolones such as cipro or doxycycline have a cure rate of 50% to 80%. Ampicillin and tetracycline may be less effective in treating an infection because many types of bacteria have become resistant to these older antibiotics. Recent research shows that 30% of mycoplasmas are resistant to tetracyclines. Cipro or doxycycline are often used for severe or complicated infections. These antibiotics cost more than other types but experts believe fluoroquinolones may have a higher cure rate because they are better at penetrating the prostate.
How long do I take the cipro or doxycycline antibiotics to treat prostatitis ?
Many studies show that a 14 day course of antibiotics can return PSA levels to normal levels but most experts recommend 3-4 weeks of treatment. Longer courses of therapy may be needed. If acute prostatitis is caught early enough, your doctor will most likely prescribe a month-long regiment of antibiotics to fight off the infection and their partners have to take the same antibiotics for a much shorter duration, usually 10-14 days. If your infection has progressed too far, you may be admitted to a hospital and placed on intravenous antibiotics. If your prostatitis is extremely painful, talk to you doctor about painkillers to help you along until the antibiotics take effect. Chronic prostatitis is treated with cipro or doxycycline antibiotics as well, only the treatment lasts much longer -- usually three months. Unfortunately, only 50 to 70 percent of men are cured. To help with the pain, your doctor may give you a non-steroidal anti-inflammatory medication to take with your antibiotics.
A normal prescription of cipro would consist of 1, 500mg tablet every 12 hours (2x daily). You would need 60, 500mg tablets of cipro to complete a 30 day regiment. Cipro may be taken with or without food. It is preferable to take cipro 2 hours after a meal. Do NOT take this medicine with milk, yogurt, or calcium-enriched orange juice. Take each dose with a full glass of water (8 ounces). Take ciprofloxacin at evenly spaced 12 hour intervals. Take all of the ciprofloxacin that has been prescribed for you even if you begin to feel better. Your symptoms may start to improve before the infection is completely treated.
The most common doxycycline regiment prescribed by doctors would consist of 1, 100mg capsules every 12 hours (2x daily). You would need 60, 100mg capsules to complete a 30 day regiment. Take each dose with a full glass of water (8 ounces). Doxycycline may be taken with food or milk or on an empty stomach. Take all of the doxycycline that has been prescribed for you even if you begin to feel better. Your symptoms may start to improve before the infection is completely treated. Do NOT take antacids that contain magnesium or aluminum (e.g., Tums or Rolaids), the ulcer medicine sucralfate (Carafate), or vitamin or mineral supplements that contain iron or zinc for a minimum of 6 hours before or 2 hours after a dose of doxycycline. Taking antacids, sucralfate, or vitamin or mineral supplements too close to a dose of doxycycline can greatly decrease the effects of the antibiotic.
How can prostatitis be prevented ?
The best prevention for prostatitis -- chronic or acute -- is to keep bacteria from getting into your urethra and causing infection in the first place. Use a condom for oral and anal sex, don’t put unsterile objects, including sex toys, into your urethra, and if you have urethritis or a urinary tract infection, see your doctor for treatment before it develops into something worse. Some doctors believe that fluids from your prostate can build-up and become an excellent place for bacteria to grow. Since these fluids are part of your semen, a good way to prevent this build-up is to ejaculate at least every other day to drain your prostate. Now that's a prescription most men can handle !